What Is Progressive Supranuclear Palsy (PSP)?

Progressive supranuclear palsy is a very rare disease affecting fine motor skills, cognition and emotions, among other things. For example, people who suffer from it may have difficulty moving, their balance and speaking.
Steele, Richardson and Olszewski discovered the disease in 1964. This is also why it is also known as Steele-Richardson-Olszewski syndrome.
As mentioned, this condition is so rare that it affects only about six in every 100,000 people. This means that it has also been very little researched. So we don’t know much about it. Unfortunately, that also means that its treatment is still not very accurate.
Progressive supranuclear palsy (PSP)
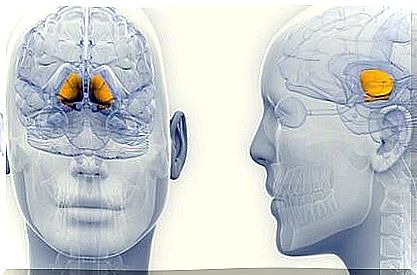
Jiménez-Jiménez (2008) defined the condition as a neurodegenerative disease, which causes a build-up of neurofibrillary tangles in the neurons and glial cells. As a result, these areas are slowly but surely starting to shrink. Ultimately, as a result, they are no longer able to send messages to the frontal lobe.
Until scientists do more research, we won’t really know what causes it. The two known theories so far are genetic as well as potential environmental factors.
The clinical picture
Progressive supranuclear palsy affects the brain in many different ways. Ardeno, Bembibre, and Triviño (2012) summarize some of its implications as follows:
- Impairment of fine motor skills. This includes gait disturbances, postural instability and Parkinson’s disease.
- We also see eye abnormalities and eyelid disorders.
- Cognitive and behavioral disorders, such as apathy, depression and social isolation.
- Pseudobulbar affect, also called emotional incontinence. This is an emotional disorder that can cause uncontrollable outbursts of emotions such as laughing or crying.
Variations
In 1994 Lantos described three different forms of progressive supranuclear palsy as follows:
- Frontal PSP causes cognitive and behavioral problems, among other things.
- The classic variant of PSP is characterized, among other things, by problems with posture, eye paralysis and pseudobulbar affect.
- Parkinson’s variation is accompanied by akinetic-rigid symptoms.
Diagnosis
This disease is usually not diagnosed until after death. This is because it is very difficult to diagnose someone while they are still alive, also because the condition is so rare. The lack of research on this disease also causes doctors to often confuse this disease with other conditions.
Therefore, most physicians today make differential diagnoses of Parkinson’s, multiple system atrophy, corticobasal degeneration, frontotemporal dementia, and Lewy body dementia. Some of the tools doctors use to diagnose this disease include:
- MRI scans
- single-photon emission computed tomographies
- positron emission tomography
According to both the National Institute of Neurological Disorders and Stroke and the Progressive Supranuclear Palsy Association , there are several diagnostic criteria for this condition.

Possible progressive supranuclear palsy
- gradually progressive disorder that begins when the individual is 40 years of age or older
- during the first year of impairment, vertical supranuclear palsy or vertical saccades occur with instability and falls
- no evidence of other diseases to explain the clinical features
Probable progressive supranuclear palsy
- proximal muscle weakness is greater than distal akinesia or stiffness
- abnormal neck position, especially bending the head back
- poor or no response to Levodopa treatments
- early swallowing disorder and dysarthria
- early cognitive impairment with at least two of the following symptoms:
- apathy
- reduction in the ability to think abstractly
- decreased verbal fluency
- imitative behavior
- primitive reflexes (called “frontal release signs”)
Definitive progressive supranuclear palsy
- history of probable or possible PSP
- histopathological evidence typical of the disease
- premature cognitive decline, along with at least two of the following symptoms:
- apathy
- decreased verbal fluency
- problems with abstract thinking
- imitative behavior
- front release signs
Evaluation
Because this disease is so rare, we don’t have a standard way of assessing it. Thus, physicians must make case-by-case evaluations. They should also use different tests and questionnaires with each patient.
Arnedo, Bembibre and Triviño (2012) published an article on the evaluation of one specific patient. They also described the resources they used. These included the following:
Attention
- Trail Making Test
- to count
- the A-test
- color blindness test
Language
- the Boston Naming Test
- semantics and phonetics
- interviews
- language evaluation
Memory
- numerical test (WAIS-III)
- Spatial Span (WMS-III),
- the Rey-Osterrieth complex number test
Executive functions
- a matrix subtest (WAIS-III)
- match test (WAIS-III)
- the Wisconsin Card Sorting Test
Visual-perceptual skills
- a battery of visual perception tests
Praxia
- the Rey-Osterrieth complex number test
- WAIS-III
- common transitive and intransitive movements
- a movement sequence
- the ability to use objects
Processing Speed:
- time-limited tests
Psychopathological Rating Scales
- a neuropsychiatric inventory
Functional scales
- the Barthel index
- the Lawton-Brody . scale

Treatment and conclusion
In conclusion, we can state that there is not yet an effective, concrete treatment for progressive supranuclear palsy. All we can do now is control the patients’ symptoms so they can live their lives.
Since we don’t know how to treat it, the goal is to slow it down and help the patient remain as independent as possible. Several specialists are involved in the treatment, including neurologists, psychologists and physiotherapists. Doctors can prescribe medications such as:
- L-DOPA
- fluoxetine
- amitryptiline
- imipramine
Certain patients also do speech therapy, cognitive stimulation therapy, and occupational therapy.